- Platform
- Solutions
-
-
Patient / Member 360
Gain a holistic view of each patient or member with WellStack’s integrated data platform, driving better health outcomes and personalized care.
Decision Hubs
Empower your organization with centralized, actionable insights through WellStack’s Decision Hubs, enabling data-driven decision-making across all levels.
Population Health management
Optimize health strategies and improve population outcomes using WellStack’s Navigate Platform for comprehensive population health management
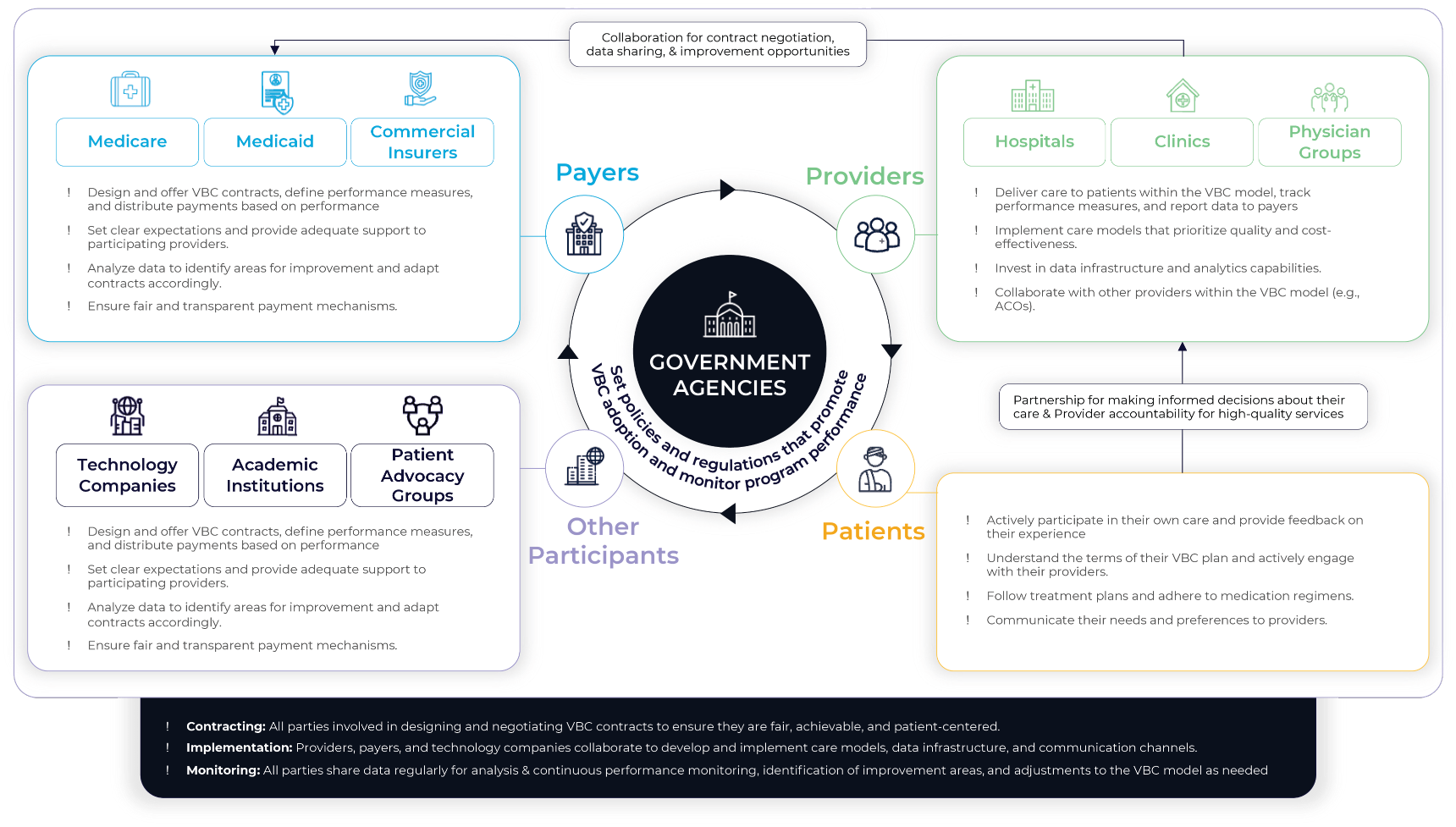
Accountable Care Organizations
Achieve coordinated and efficient healthcare delivery with WellStack’s solutions designed for accountable care organizations, focusing on value and quality.
Value Based Care
Transition to a value-based care model with WellStack’s comprehensive solutions that prioritize outcomes and cost-efficiency.
AI/ML Enablement
Leverage advanced AI and ML capabilities with WellStack’s solutions to drive innovation and improve clinical and operational outcomes.
WellStack Labs
Your sandbox for next-gen healthcare innovation
-
-
- Services
- Data Pioneers
- About Us
-
-
Company
Discover WellStack’s mission to transform healthcare through advanced data integration and analytics, empowering providers to deliver superior patient care.
Insights
Explore a range of articles that delve into the latest innovations, trends, & strategies in healthcare data management from WellStack’s industry experts
News
Stay updated with the latest developments, product launches, and healthcare innovations from WellStack, a leader in healthcare technology solutions.
Partnerships
Learn about WellStack’s strategic partnerships that enhance our capabilities and extend our reach in the healthcare industry, fostering collaborative solutions.
Case Studies
Explore detailed case studies highlighting how WellStack’s cutting-edge solutions have driven success and innovation in healthcare organizations.
Thought Leadership
Dive into insights from WellStack’s experts who are at the forefront of reshaping healthcare with forward-thinking strategies and pioneering research.
Careers
Empower Your Career. Transform Healthcare. Grow with WellStack
-
- How To Buy